14
Oct
Research Bill Would Support Organic Sector, Seen as Solution to Health and Environmental Crises
(Beyond Pesticides, October 14, 2025) With escalating environmental, health, climate crises tied to petrochemical pesticides and fertilizers, Beyond Pesticides is calling the transition to organic land management a mandate, not a choice. Additionally, as a solution, organic agriculture has returned competitive yields with chemical-intensive farming and higher profitability. In the context, the Beyond Pesticides and its network is supporting the Organic Science and Research Investment (OSRI) Act, S.1385 and H.R. 5703, to help grow the organic sector and asking members of Congress to cosponsor the legislation. If passed, OSRI will make strategic investments into the U.S. Department of Agriculture’s (USDA) organic agriculture research, assisting farmers to meet the growing demand for organic products and keep organic dollars circulating in rural and regional economies. The House and Senate bills include the same legislative language.Â
As the health, biodiversity, and climate crises escalate, Beyond Pesticides views organic agriculture and nonagricultural land management as a social good, necessary to a sustainable future. Given the dismantling of many federal environmental programs and the weakening or undermining of pesticide regulation, the transition to organic alternative has taken on increased importance, according to public health and environmental advocates. The true cost of conventional, petrochemical pesticide and fertilizer use is integral to any calculation of the overall economic benefit of organic practices. Most of the costs of chemical-intensive land management are not borne by the pesticide user or chemical companies, but by society or taxpayers who bear the cost of environmental and human health harms, lost ecosystem services such as die-off of pollinators, water contamination, and the cost of fighting climate-induced fires and flooding.Â
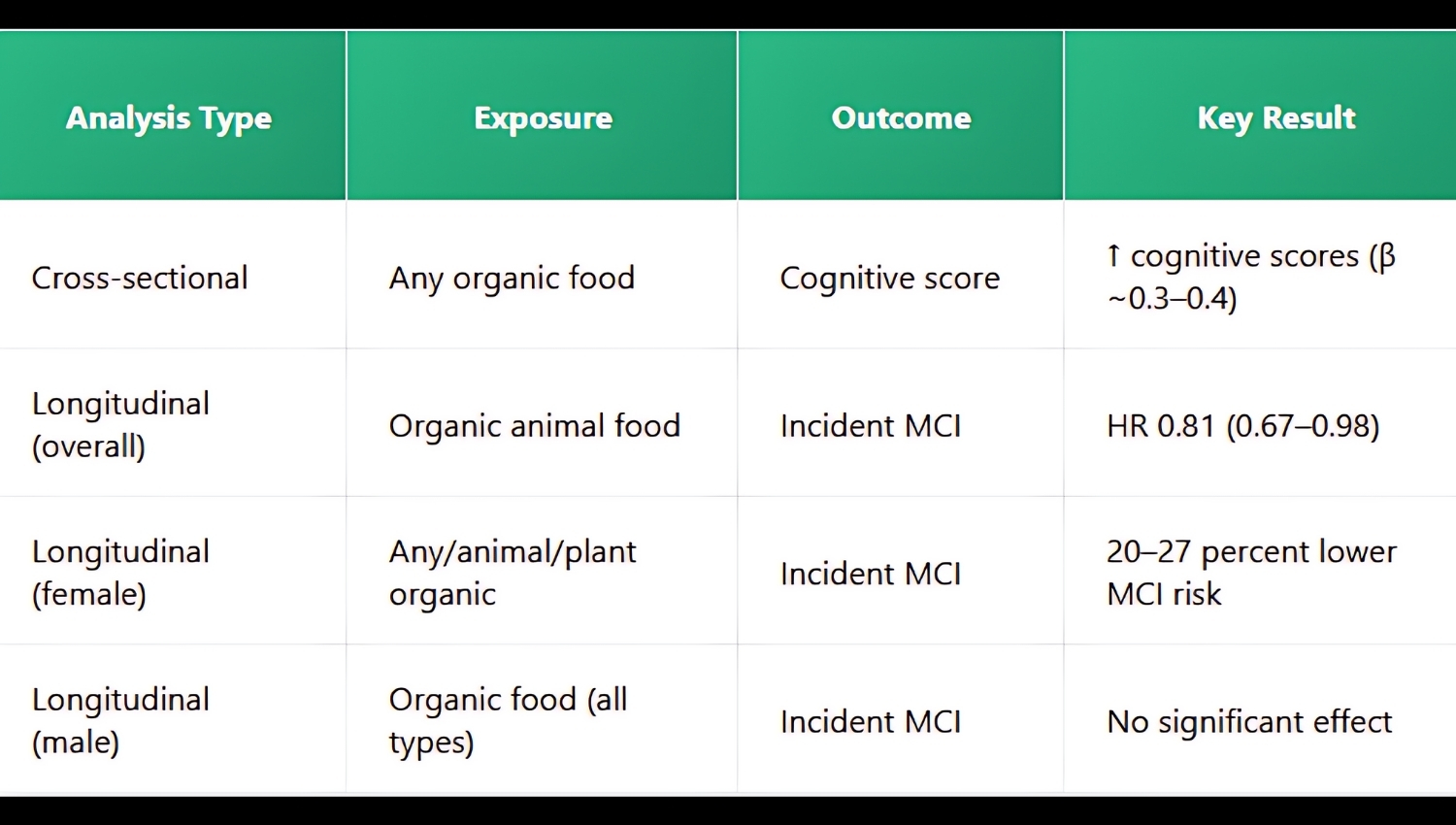
Research in recent months finds: consumption of organic animal-based and plant-based foods is positively associated with higher cognitive scores; organic rice paddies in the Mediterranean region have greater ecosystem biodiversity than their chemical-intensive counterparts; âorganic farming equals conventional yield under irrigation and enhances seed quality in drought, aiding food security;â organic corn outcompetes with chemical-intensive corn in Kenya; organic agriculture fosters insect biodiversity that provides ecosystem services like pollination and biocontrol; and, organic grain cropping systems contain higher concentrations of total nitrogen and soil organic carbon, exceeding those found in chemical-intensive systems.Â
OSRI (H.R. 5703) was introduced in the U.S. House of Representatives on October 6 by Representative Eugene Vindman (D-VA), with co-sponsor Michael Lawler (R-NY), and reintroduced in the U.S. Senate (S.1385) in April by sponsors John Fetterman (D-PA) and Sen. Adam Schiff (D-CA), and cosponsors Kirsten Gillibrand (D-NY), Cory Booker (D-NJ), Jeff Merkley (D-OR), Tammy Baldwin (D-WI), Tina Smith (D-MN), Peter Welch (D-VT), Alex Padilla (D-CA), Ron Wyden (D-OR), and Angus King (I-ME). The legislation seeks to ensure âorganics research is prioritized at the U.S. Department of Agriculture (USDA) and [increased] funding for research agencies and universities, [as well as ] provid[ing] much needed support to the organic farming industry.âÂ
Specifically, OSRI strengthens federal commitments to organic agriculture by:Â
- Creating the Coordinating and Expanding Organic Research Initiative at the USDA to assess and efficiently expand the agency’s organic research portfolio.Â
- Increasing funding for the Organic Research and Extension Initiative (OREI) from its current budget of $50 million annually to $100 million by the end of the next Farm Bill.Â
- Formally authorizing the Organic Transition Research Program to support farmers transitioning to organic practices, renaming the program to the Researching the Transition to Organic Program (RTOP).Â
- Doubling Farm Bill support for the Organic Production and Market Data Initiative to improve market transparency, help inform targeted market development investments, and improve risk management tools.Â
- Directing the USDA’s Economic Research Service to evaluate the full economic, ecological, and community impacts of organic agriculture.Â
At a time when food security and economic resilience are more important than ever, OSRI helps ensure that U.S. producers, not foreign suppliers, are meeting the needs of American consumers.Â
Letter to U.S. Congress
A growing body of evidence demonstrates the environmental, health, climate, and economic benefits of organic agriculture. As crises escalate, organic agriculture and nonagricultural land management must be viewed as a social good, necessary to a sustainable future. Societal transition to organic practices requires a reorientation to its value as a public good. Given the dismantling of many federal environmental programs and weakening or undermining of pesticide regulation, it is critical to support the organic alternative. The true cost of conventional, petrochemical pesticide and fertilizer use is integral to any calculation of the overall economic benefit of organic practices. Most of the costs of chemical-intensive land management are not borne by the pesticide user or chemical companies, but by society or taxpayers who bear the cost of environmental and human health harms, lost ecosystem services such as die-off of pollinators, water contamination, and the cost of fighting climate-induced fires and flooding.Â
Research in recent months finds: consumption of organic animal-based and plant-based foods is positively associated with higher cognitive scores; organic rice paddies in the Mediterranean region have greater ecosystem biodiversity than their chemical-intensive counterparts; âorganic farming equals conventional yield under irrigation and enhances seed quality in drought, aiding food security;â organic corn outcompetes chemical-intensive corn in Kenya; organic agriculture fosters insect biodiversity that provides ecosystem services like pollination and biocontrol; and organic grain cropping systems contain higher concentrations of total nitrogen and soil organic carbon, exceeding those found in chemical-intensive systems.
Fortunately, members of the U.S. House of Representatives and Senate have reintroduced the Organic Science and Research Investment (OSRI) Act, S.1385 and H.R. 5703, which will make strategic investments into USDA organic agriculture research, assisting farmers to meet the growing demand for organic products and keep organic dollars circulating in rural and regional economies.
In April, Senators John Fetterman (PA-D) and Sen. Adam Schiff (CA-D), reintroduced OSRI, S.1385, to ensure âorganics research is prioritized at the U.S. Department of Agriculture (USDA) and [increased] funding for research agencies and universities, [as well as] provid[ing] much needed support to the organic farming industry.â The bill is co-sponsored by Senators Kirsten Gillibrand (D-NY), Cory Booker (D-NJ), Jeff Merkley (D-OR), Tammy Baldwin (D-WI), Tina Smith (D-MN), Peter Welch (D-VT), Alex Padilla (D-CA), Ron Wyden (D-OR), and Angus King (I-ME). Representatives Lawler (R-NY) and Vindman (D-VA) have introduced a House version, H.R. 5703.
Specifically, OSRI strengthens federal commitments to organic agriculture by:
*Creating the Coordinating and Expanding Organic Research Initiative at the USDA to assess and efficiently expand the agencyâs organic research portfolio.
*Increasing funding for the Organic Research and Extension Initiative (OREI) from its current budget of $50 million annually to $100 million by the end of the next Farm Bill.
*Formally authorizing the Organic Transition Research Program to support farmers transitioning to organic practices, renaming the program to the Researching the Transition to Organic Program (RTOP).
*Doubling Farm Bill support for the Organic Production and Market Data Initiative to improve market transparency, help inform targeted market development investments, and improve risk management tools.
*Directing the USDAâs Economic Research Service to evaluate the full economic, ecological, and community impacts of organic agriculture.
At a time when food security and economic resilience are more important than ever, OSRI helps ensure that U.S. producers, not foreign suppliers, are meeting the needs of American consumers.
Please cosponsor OSRI.
















 Â
 

