08
May
Proposed Legislation To Allow Massachusetts to Blanket State with Mosquito Pesticides that Attack the Immune and Respiratory Systems, During a Pandemic that Attacks the Same Systems
 (Beyond Pesticides, May 8, 2020) At the height of Covid-19 impacts in the Northeast U.S., Massachusetts Governor Charlie Baker (R) and Lieutenant Governor Karyn Polito (R) filed emergency legislation at the Boston State House that would, according to their April 16 press release, âhelp the Commonwealth more effectively combat diseases transmitted by mosquitoes, including arboviruses like Eastern Equine Encephalitis (EEE) and West Nile Virus (WNV), by authorizing a coordinated, proactive, statewide approach to mosquito control activities.â Protecting the public from such diseases is an important public health mission. However, the Governorâs bill, H.4650, represents an alarming âover-reachâ that would give unitary authority to the State Reclamation and Mosquito Control Board (SRMCB) to conduct mosquito control activities, including ineffective and toxic spraying, with virtually no effective oversight or transparency. Beyond Pesticides opposes this bill, whose passage would enable use of pesticides that can have respiratory and immune impacts â increasing health risks for everyone, but especially for the many people already at higher risk from Covid-19, despite the availability of ecological management approaches that eliminate the need for toxic chemicals.
(Beyond Pesticides, May 8, 2020) At the height of Covid-19 impacts in the Northeast U.S., Massachusetts Governor Charlie Baker (R) and Lieutenant Governor Karyn Polito (R) filed emergency legislation at the Boston State House that would, according to their April 16 press release, âhelp the Commonwealth more effectively combat diseases transmitted by mosquitoes, including arboviruses like Eastern Equine Encephalitis (EEE) and West Nile Virus (WNV), by authorizing a coordinated, proactive, statewide approach to mosquito control activities.â Protecting the public from such diseases is an important public health mission. However, the Governorâs bill, H.4650, represents an alarming âover-reachâ that would give unitary authority to the State Reclamation and Mosquito Control Board (SRMCB) to conduct mosquito control activities, including ineffective and toxic spraying, with virtually no effective oversight or transparency. Beyond Pesticides opposes this bill, whose passage would enable use of pesticides that can have respiratory and immune impacts â increasing health risks for everyone, but especially for the many people already at higher risk from Covid-19, despite the availability of ecological management approaches that eliminate the need for toxic chemicals.
H.4650, An Act to mitigate arbovirus in the Commonwealth â was promulgated in response to a Massachusetts Department of Public Health (DPH) determination that 2020 may bring mosquito-borne arboviruses â which can cause diseases, such as EEE and WNV â to the state, although at what levels and where are now neither known nor predictable. The state saw 12 human cases of EEE and four deaths from the rare infection in 2019; EEE was also confirmed in nine livestock animals. Outbreaks of EEE typically last for two or three years.
Most people who contract EEE have either no or mild symptoms (e.g., fever, joint or muscle ache), but severe infections can cause swelling of the brain (encephalitis) or meninges (meningitis), as well as flu-like symptoms. In some cases, seizures or coma may ensue; approximately one-third of people who develop encephalitis with EEE die, and some who do survive have significant neurological disabilities. West Nile Virus is asymptomatic in many people, and may cause illness in roughly 20% of those infected, with 1.5% of people developing serious illness (and occasionally, dying from WNV).
Despite the extraordinary power given to the state board in this legislation to engage in âeradication methods as it deems necessary in any area of the Commonwealth,â experts are clear that surveillance for arboviruses is critical to defining a restrained program that does not engage in widespread spraying. More critically, effective mosquito management integrates rigorous monitoring and surveillance, elimination of breeding sites, enhancing habitat for mosquito predators, biological controls of mosquito larvae, and public education. The absence of monitoring of arboviruses in parts of the state that do not belong to regional mosquito control districts means there is inadequate data on the presence of the viruses in mosquito populations â making it difficult to develop risk assessments and plan mitigation activities. The SRMCB oversees all mosquito control activities in Massachusetts, including those conducted by regional mosquito control districts and projects, but at present has no authority to conduct mosquito control activities independently in communities that do not belong to a mosquito control district. Â
Notably, the bill itself is unusually â and perhaps alarmingly â brief. This is the entire text of H.4650 (the first paragraph is an âEmergency Preambleâ):
âWhereas, The deferred operation of this act would tend to defeat its purpose, which is forthwith to make a certain change in law to allow the Commonwealth to immediately respond to the significant public health risks associated with the transmission of arbovirus from mosquitoes to humans, such change being immediately necessary to carry out to accomplish important public purposes, therefore it is hereby declared to be an emergency law, necessary for the immediate preservation of the public health and convenience.
SECTION 1. Chapter 252 of the General Laws is hereby amended by inserting after section 2 the following section:
Section 2A. Notwithstanding any general or special law to the contrary and upon the written determination of the commissioner of public health that an elevated risk of arbovirus exists or may exist for the following year, the board, in consultation with the department of public health, may engage in preventative and eradication methods as it deems necessary in any area of the Commonwealth. In carrying out its authority under this section, the board may act through any district or project duly organized under this chapter, other agencies of the commonwealth [sic], and may employ other professionals as the board deems necessary. All actions taken under the authority of this section shall be designed to protect public health while minimizing to the extent feasible any adverse impact to the environment.â
Commentary and Analysis
It is difficult not to have the impression that H.4650 was assembled in great hurry and without the informed consideration more typical of proposed legislation. The critiques of the bill that follow here will provide evidence that supports that impression.
H.4650 was referred by both the Massachusetts Senate and House to the legislatureâs Joint Committee on Public Health on April 21; it is scheduled for a hearing on May 11. Senate President Karen Spilka said, in the Governorâs office press release, âI believe we need a comprehensive, coordinated, and systematic approach to tackling EEE and we must ensure that approach covers all corners of the Commonwealth.â The administration cites the need for better data, and a comprehensive approach across the state in protecting public health, which sounds reasonable enough, given the health threat represented by EEE, especially.
Beyond Pesticides, Mass Audubon, the Massachusetts Association of Conservation Commissions (MACC), and others oppose this bill, and offer a variety of critiques of it. The administrationâs press release notes that the bill would permit SRMCB to âengage in mosquito control activities across the Commonwealth . . . when the Commissioner of Public Health determines that an elevated risk of arbovirus existsâ â without setting any parameters for what âelevated riskâ means. The bill would allow the commissioner to determine âthat an elevated risk of arbovirus exists or may exist for the following year,â [emphasis by Beyond Pesticides] on which determination the SRMCB would then be able to act.
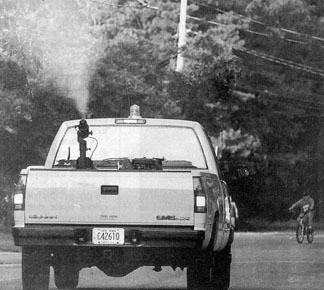
Critics expect that the bill will result in an over-reliance on insecticide spraying as a mosquito control measure. Beyond Pesticides has long maintained that spraying pesticides to kill adult mosquitoes (âadulticidingâ) is not only ineffective, but also, dangerous. The chemical pesticides used in such spraying (as well as those used in homes and gardens, and in food production) can exhibit a variety of toxic effects in humans, including compromise of respiratory and immune systems.
The most common insecticides used currently are organophosphates and pyrethroids, both of which have broad toxicity for nontarget species, including fish, birds, and amphibians. The health (and environmental) toxicity of these chemicals is a worry in ânormalâ times, but in this pandemic time, it is especially concerning because use of adulticiding chemicals elevates the risks related to infection with Covid-19 â which has harmful impacts on human immune and respiratory systems. Indeed, the only reference to potential impacts in the text of the bill is this: âAll actions taken under the authority of this section shall be designed to protect public health while minimizing to the extent feasible any adverse impact to the environment.â
The preemptive nature of the bill is also worrisome. In testimony submitted to the Joint Committee on Public Health on May 4, Mass Audubonâs Legislative Director, Michael Cusher, said that the bill supersedes the mandates of all other state statutes and special laws, including Massachusettsâs Open Meeting Law and Public Records Act â both of which serve as vehicles of transparency and accountability for the publicâs benefit. If passed, H.4650 would also trump local bylaws and regulations that may have been created to deal with such risks in a locally appropriate manner.
Beyond Pesticide has written, âSuch power, without accountability to the public and independent science, would preempt local communities from disagreeing with state-level decisions around pesticide use, and override local opt-out agreements made by private residents.â Currently, Massachusetts residents in a municipality that belongs to a regional mosquito control district can request and receive ânuisance sprayingâ on their private property at will. Residents are also able to exempt their properties from such spraying, but as many critics have complained, such exemption is relatively ineffective because sprayed pesticides can drift well off their target parcels.
Mass Audubon also warns that any number of other laws protective of human and environmental health could be âoverridden or ignored, without accountability or disclosure.â Those could include the Massachusetts Endangered Species Act, the stateâs Pesticide Control Act, and/or the Wetlands Protection, among others. A Mass Audubon Advocacy Blog entry points out that the bill has no expiration date and provides no opportunity for input on SRMCB control activities from affected communities or landowners.
Kyla Bennett, the New England Director, and Director of Science Policy, for PEER (Public Employees for Environmental Responsibility), outlined a host of reasons for opposing H.4650. Echoing many of the concerns of Beyond Pesticides, Mass Audubon, and Massachusetts Association of Conservation Commissions (MACC) (see next paragraph), the list includes:
- the bill is far too broad and represents significant over-reach
- the bill has no sunset provision
- it would pre-empt municipal decision making (e.g., not to join a regional district to avoid nuisance spraying), as well as overrule private property requests for spraying exemptions
- it does not account for environmental impacts of widespread adulticiding (or other strategies)
- it fails to address public health implications of broad-scale spraying, especially on vulnerable populations
- DPH has not undertaken any analysis of how and why EEE has achieved such geographic spread in the state
The MACC issued a May 1 legislative alert to its members setting out its opposition to the bill. It also submitted a letter to the chair of the Joint Committee on Public Health citing its concerns and recommendations for modifications. Those concerns are: (1) the breadth and pre-emptive nature of the bill, (2) the lack of transparency about how decisions would be made, and eclipse of any role for local boards of health and environmental groups, (3) the absence of requirements for community and property owner notification of control measures, (4) the lack of information or mention of either the efficacy of adulticiding or inadvertent impacts on organisms and ecosystems, and (5) the lack of a sunset provision.
MACCâs recommendations include: (1) adding DPH and Department of Fish and Game to SRMCB; (2) requiring 48-hour notification to communities prior to spraying; (3) annual reporting of plans, programs, and results, and an annual public review process; (4) requiring use of IPM (Integrated Pest Management) plans with an emphasis on surveillance, public education, and ecologically based methods; and (5) enabling communities to sign up for surveillance and data services without accompanying pesticide application services.
Beyond Pesticides and Mass Audubon agree that Massachusetts needs to reform its existing monitoring and mitigation systems, which are supposed to protect the public from risks of EEE and WNV; Mass Audubon calls them âantiquated and fragmented.â Beyond Pesticides asserts that the state should â rather than authorize SRMCB to âspray toxic pesticides anywhere in the state at any timeâ â focus on supporting local efforts to eliminate breeding sites, manage mosquito larvae through biological controls, and conduct public education on prevention strategies. Pesticide use should be considered only as a last resort. H.4650 neither suggests nor requires that such a program of safer protocols be implemented before SRMCB could implement âeradication methods as it deems necessary in any area of the Commonwealth.â
There are far better approaches than the one this legislation would enable, and resources with which to identify and implement them â for policy makers and the public â abound. Legislators and executives can avail themselves of the 2012 Beyond Pesticides and National Coalition Against the Misuse of Pesticides publication, Public Health Mosquito Management Strategy for Decision Makers and Communities, a comprehensive guide to effective and safe mosquito control for public health strategies. The Xerces Society offers How to Help Your Community Create an Effective Mosquito Management Plan. Beyond Pesticides provides online resources on its Resources page and its Tools for Change page, which provides factsheets, position statements, and organizing tips for local communities.
Beyond Pesticides issued a May 7 Action Alert on this bill for Massachusetts residents. If you live in Massachusetts, please use it to add your voice in opposing H.4650 and advocating for an approach that is more effective, less sweeping in its reach, and safer for residents of the Commonwealth, especially during this pandemic.
All unattributed positions and opinions in this piece are those of Beyond Pesticides.
Sources: https://www.mass.gov/news/baker-polito-administration-files-legislation-to-combat-mosquito-borne-diseases-in-the and https://malegislature.gov/Bills/191/H4650
Â
Â
Â
Â








 (Beyond Pesticides, May 6, 2020) The coronavirus pandemic highlights pre-existing cracks in social safety nets and environmental regulation. Pollutants, such as respiratory and immune-suppressing toxic pesticides,
(Beyond Pesticides, May 6, 2020) The coronavirus pandemic highlights pre-existing cracks in social safety nets and environmental regulation. Pollutants, such as respiratory and immune-suppressing toxic pesticides, 
 (Beyond Pesticides, May 4, 2020)Â Exemptions to the Fair Labor Standards Act allow children to work unlimited hours in agriculture at the age of 12 and allow child farmworkers to perform hazardous work at the age of 16. These exemptions apply only to farm labor and areÂ
(Beyond Pesticides, May 4, 2020) Exemptions to the Fair Labor Standards Act allow children to work unlimited hours in agriculture at the age of 12 and allow child farmworkers to perform hazardous work at the age of 16. These exemptions apply only to farm labor and are 





 In 1962, Rachel Carson said we stood at a crossroads:
In 1962, Rachel Carson said we stood at a crossroads: >>Tell EPA Administrator Andrew Wheeler to follow the advice of scientists and do his job. Tell your Congressional representatives to support scientific integrity at EPA and other agencies.
>>Tell EPA Administrator Andrew Wheeler to follow the advice of scientists and do his job. Tell your Congressional representatives to support scientific integrity at EPA and other agencies. P-22 is being treated for mange; blood tests found anti-coagulant rodenticides, commonly known as rat poison.
P-22 is being treated for mange; blood tests found anti-coagulant rodenticides, commonly known as rat poison.

 (Beyond Pesticides, April 16, 2020) Pesticide exposure in farmland birds is a concomitant of pesticide-treated muesli (cereal) seed commonly planted during winter months, according to researchÂ
(Beyond Pesticides, April 16, 2020) Pesticide exposure in farmland birds is a concomitant of pesticide-treated muesli (cereal) seed commonly planted during winter months, according to research  (Beyond Pesticides, April 15, 2020) Home pesticide use during pregnancy is associated with an increased risk of a child developing the kidney cancer nephroblastoma, or Wilmsâ tumor, according to
(Beyond Pesticides, April 15, 2020) Home pesticide use during pregnancy is associated with an increased risk of a child developing the kidney cancer nephroblastoma, or Wilmsâ tumor, according to  (Beyond Pesticides, April 14, 2020)Â An op-ed in theÂ
(Beyond Pesticides, April 14, 2020) An op-ed in the  (Beyond Pesticides, April 13, 2020) Since 1990, Congress has required an every-five-years review of its Dietary Guidelines â recommendations that are supposed, minimally, to promote public health and prevent chronic diseases. The next review and a draft updated iteration, the
(Beyond Pesticides, April 13, 2020)Â Since 1990, Congress has required an every-five-years review of its Dietary Guidelines â recommendations that are supposed, minimally, to promote public health and prevent chronic diseases. The next review and a draft updated iteration, the  (Beyond Pesticides, April 9, 2020) Brazilian tax exemptions benefit the agrichemical industry to the tune of $2.2 billion USD annually, according to researchers from the Oswaldo Cruz foundation and the Federal Rural University of Rio de Janeiro. ABRASCO, the Brazilian Association of Collective Health, headed a new study which illuminates a tight relationship between Brazilian government and industry. Researchers additionally point to millions of dollars given from public resource funds to the companies. While industry lobby groups argue that toxic pesticides are necessary for development and food production, environmental and health advocates say the people of Brazil bear the brunt of toxic pesticide contamination while international companies profit.
(Beyond Pesticides, April 9, 2020) Brazilian tax exemptions benefit the agrichemical industry to the tune of $2.2 billion USD annually, according to researchers from the Oswaldo Cruz foundation and the Federal Rural University of Rio de Janeiro. ABRASCO, the Brazilian Association of Collective Health, headed a new study which illuminates a tight relationship between Brazilian government and industry. Researchers additionally point to millions of dollars given from public resource funds to the companies. While industry lobby groups argue that toxic pesticides are necessary for development and food production, environmental and health advocates say the people of Brazil bear the brunt of toxic pesticide contamination while international companies profit. (Beyond Pesticides, April 9, 2020) Honey bees (Apis mellifera) remain in severe decline, with U.S. beekeepers losing
(Beyond Pesticides, April 9, 2020) Honey bees (Apis mellifera) remain in severe decline, with U.S. beekeepers losing 

